About PRP
Harnessing the power of your body’s own natural healing abilities.
Our blood plasma treatments offer a gentle yet highly effective way to rejuvenate and restore yourself.
Our Autologous Regenerative Therapies
View our collection of regenerative treatments which uses advanced techniques to refresh and restore you at a cellular level.
A natural treatment that uses your own blood to isolate platelets, which are rich in natural growth factors.
When reintroduced to targeted areas, PRP stimulates tissue repair, supports collagen production, and enhances cell renewal.
Commonly used in aesthetics for skin rejuvenation, hair restoration, and healing support.
An advanced form of PRP which contains a natural fibrin matrix. PRF allows growth factors and healing cells to be released slowly over time, supporting longer-lasting regeneration with the benefits of more sustained results.
It is commonly used for skin rejuvenation, under-eye & lip treatments, and hair restoration.
A refined & purified preparation is a purified preparation that isolates highly active growth factors. These growth factors play a key role in stimulating cellular activity and regeneration.
In aesthetics, GFC is used to address hair thinning, skin aging, and overall tissue revitalisation.
Nano-sized cell-derived messengers that deliver proteins, lipids, and genetic material to support cellular communication and repair.
They offer benefits such as enhanced cell renewal, reduction of inflammation, and promotion of a balanced environment.
The Method

Step 1
Take blood
Where science meets natural beauty & restoration
Platelet-Rich Plasma (PRP) therapy has become one of the most demanding regenerative treatments in aesthetic medicine. Whether it’s used for facial rejuvenation, hair restoration, or tissue repair, PRP relies on the body’s own healing physiology to stimulate natural repair and regeneration. But what’s really happening beneath the surface? Let’s break down the science.
PRP is an autologous blood concentrate, meaning it’s derived from your own blood. After your blood is drawn, the sample is placed in a centrifuge to separate its components by density. This process concentrates the platelets cells that play a central role in wound healing, into a plasma solution. The plasma contains 3–5 times more platelets than normal blood.
This results in a potent mixture rich in growth factors, cytokines, and bioactive proteins that stimulate tissue repair and regeneration.
1. Platelet Activation & Degranulation
Once injected into the skin or scalp, the platelets contact cellular signals to become activated. This activation triggers degranulation, a process where platelets release a cascade of growth factors from their alpha granules. Key molecules include:
Platelet-Derived Growth Factor (PDGF): Stimulates cell proliferation and angiogenesis (new blood vessel formation).
Transforming Growth Factor-beta (TGF-β): Regulates inflammation and promotes collagen synthesis.
Vascular Endothelial Growth Factor (VEGF): Encourages new capillary growth, improving oxygen and nutrient supply.
Epidermal Growth Factor (EGF): Enhances cell turnover and tissue remodeling.
Insulin-Like Growth Factor (IGF): Supports fibroblast activity and extracellular matrix production.
Together, these molecules create a microenvironment of regeneration, promoting the body’s intrinsic healing response.
2. Cellular Recruitment & Tissue Re-modelling
After the growth factors are released, local fibroblasts, keratinocytes, and stem cells are recruited to the injection site. These cells synthesise new collagen, elastin, and extracellular matrix proteins, which are key components that restore skin firmness and elasticity.
In the scalp, PRP stimulates dermal papilla cells in hair follicles, extending the anagen (growth) phase and promoting thicker, healthier hair shafts.
3. Angiogenesis & Improved Microcirculation
VEGF and PDGF enhance angiogenesis, forming new micro-vessels that deliver oxygen and nutrients to regenerating tissue. This not only supports healing but also improves blood circulation and metabolic activity.
4. Healing & Results
PRP doesn’t work like a filler — it’s biological regeneration, not mechanical alteration. The growth factors released by platelets only initiate healing; the real structural changes come from your body’s own cellular response, which naturally unfolds over weeks to months.
Facial PRP:
Mild glow can appear within a few days.
Noticeable textural and tone improvements occur around 4–6 weeks.
Peak results: 3–6 months post-treatment as collagen remodels.
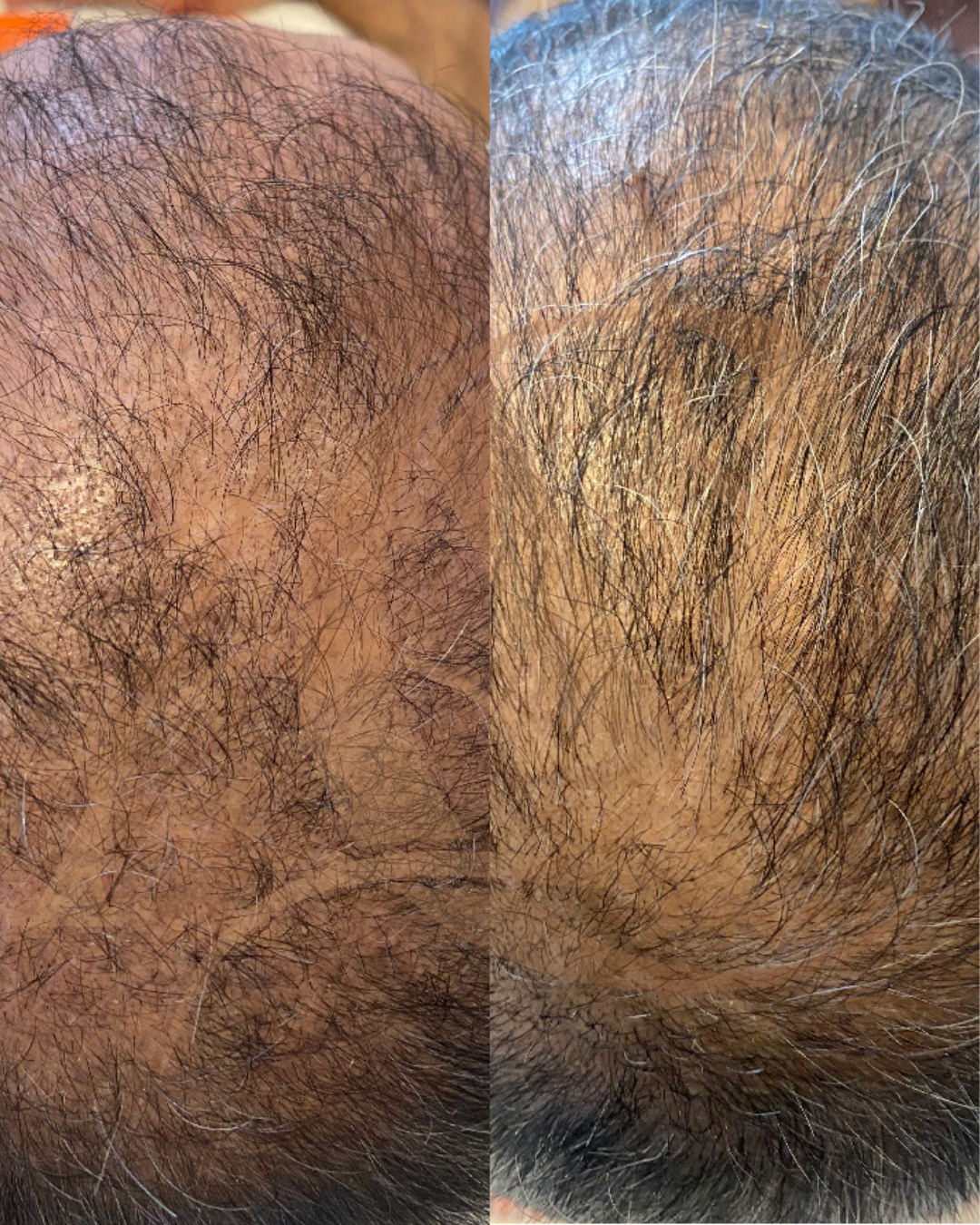
Hair PRP:
Reduced shedding can appear by 1 month.
New hair growth typically visible around 3 months.
Optimal density at 6–12 months, especially with a series of sessions.
PRP for joint or soft-tissue healing:
Pain and inflammation often improve after 2–4 weeks.
Structural tissue changes (e.g. tendon repair) continue for months.
Platelet Concentration
Normal whole blood contains approximately 150,000–350,000 platelets per microliter (µL).
After centrifugation, PRP typically concentrates those platelets by 3–5 times the baseline value
However, this can vary depending on the centrifuge system, spin speed, and volume collected.
At Aesthetics Central we draw ~20ml of blood prior to centrifugation.

Active Phase
Once PRP is activated (by exposure to tissue collagen, thrombin, calcium chloride, or injury at the injection site), the platelets begin releasing their bioactive molecules almost immediately. This release occurs in two phases:
PHASE 1: Immediate (0–10 minutes)
Upon activation, the α-granules in the platelets release ~70% of their stored growth factors within the first 10 minutes.
Key cytokines and growth factors such as PDGF, TGF-β, and VEGF flood the local environment, triggering the body’s repair cascade.
PHASE 2: Sustained Release (up to 7 days)
The remaining 30% of growth factors are gradually secreted over the next 5–7 days as the platelets continue to degranulate and then degrade.
During this time, local fibroblasts, endothelial cells, and stem cells respond by increasing and synthesising new matrix proteins (like collagen and elastin).
TISSUE REMODELING:
While the active biochemical phase lasts about a week, collagen remodeling and angiogenesis continue for weeks to months after treatment.
This is why aesthetic improvements (like smoother skin or stronger hair regrowth) become more visible over 4–12 weeks.
Aesthetic
Skin Rejuvenation
Mechanism
- Stimulates fibroblasts and boosts collagen formation.
Benefits
- Improves tone, texture, and elasticity; reduces fine lines and wrinkles.
Hair Restoration
Mechanism
- Activates dermal papilla cells, prolonging the hair growth (anagen) phase.
Benefits
- Less shedding, thicker shafts, and visible regrowth within months.
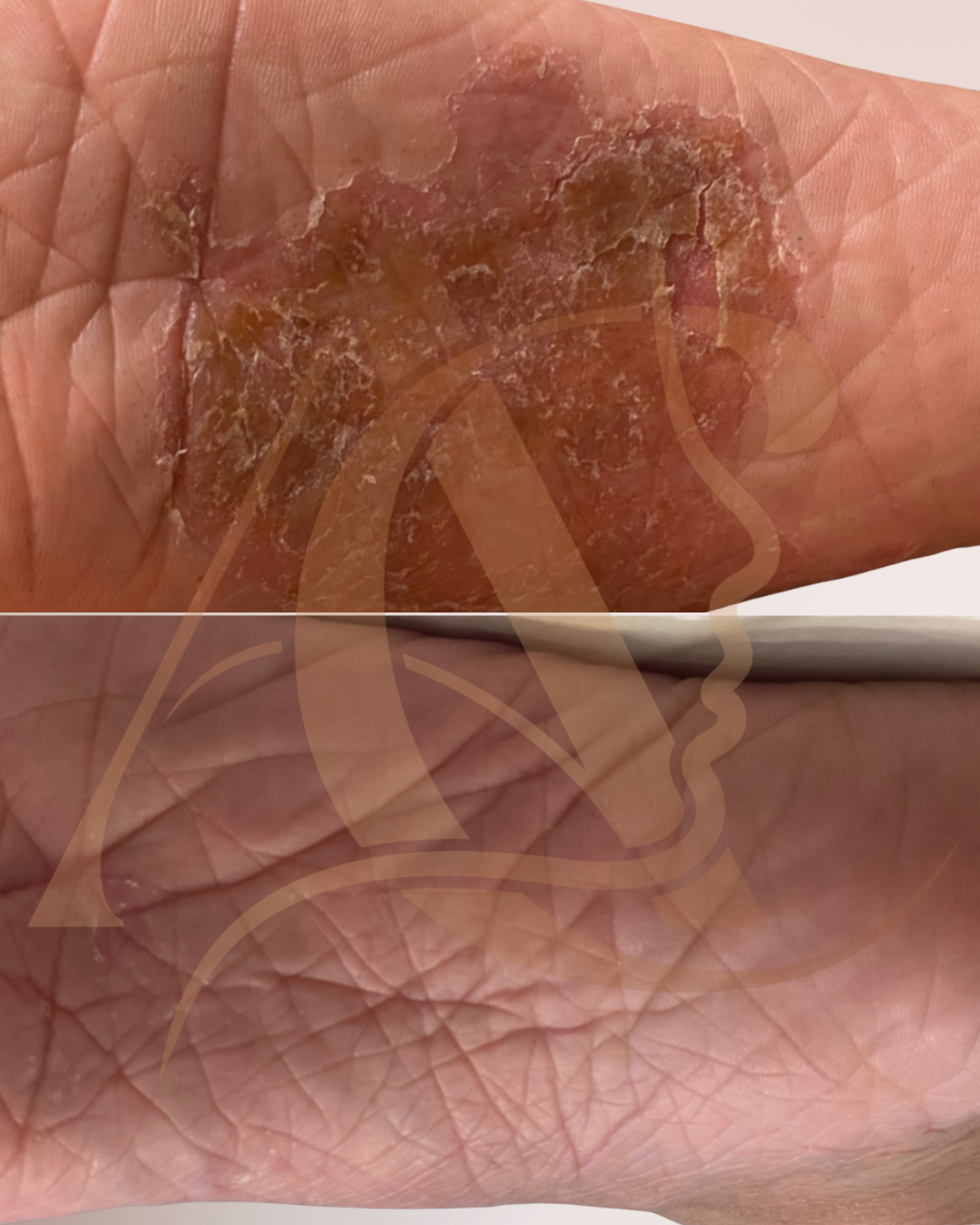
Scar & Acne Scar Treatment
Mechanism
- Remodels collagen and accelerates wound healing.
Benefits
- Smoother skin, improved texture, and softened scars.
Gynaecologic
O-Shot® (Orchid Shot)
Mechanism
- PRP is injected into specific areas of the vaginal and clitoral tissue. The platelets release growth factors that stimulate new blood vessel formation, nerve regeneration, and mucosal rejuvenation.
Benefits
Enhanced sexual sensitivity and arousal
Improved vaginal lubrication and tissue tone
Reduction in stress urinary incontinence symptoms
Support for post-menopausal vaginal dryness or discomfort
Potential aid in orgasmic function and overall sexual confidence
Orthopedic
Tendon and Ligament Injuries
Examples
- Tennis elbow, Achilles tendinopathy, rotator cuff injuries
Benefits
Reduces pain and inflammation
Promotes faster tendon healing
Decreases need for corticosteroid injections
Osteoarthritis
Mechanism
- PRP modulates inflammatory cytokines and supports cartilage matrix regeneration.
Benefits
Reduces joint pain and stiffness
Improves mobility and function
Potential disease-modifying effect on early OA
Platelet-Rich Fibrin(PRF) is an advanced evolution of Platelet-Rich Plasma (PRP), both of which harness the body’s own healing properties for skin rejuvenation and tissue repair. Like PRP, PRF is created by drawing a small amount of your blood and centrifuging it to separate the natural growth factors and platelets. However, PRF is spun at a lower speed without anticoagulants, resulting in a fibrin matrix that releases growth factors more slowly and naturally over time. This makes PRF a 100% autologous, chemical-free treatment that promotes collagen production, enhances skin texture, and supports long-term tissue regeneration — offering a more natural and sustained approach to aesthetic rejuvenation than traditional PRP.
The fibrin matrix entraps platelets, leukocytes, and circulating stem cells. This 3D fibrin scaffold allows for the sustained release of growth factors such as platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), and vascular endothelial growth factor (VEGF) over several days, enhancing angiogenesis, collagen synthesis, and tissue regeneration.
Discover how Platelet-Rich Fibrin (PRF) naturally rejuvenates the skin. Learn the science behind PRF, and why it is a superior treatment for collagen stimulation and skin regeneration in modern aesthetic medicine.
1. Blood Collection & Centrifugation
A small amount of the patient’s blood is drawn and centrifuged at a lower speed and shorter duration than PRP.
This gentle process preserves more platelets, leukocytes, and mesenchymal stem cells in a fibrin-rich plasma layer.
2. Formation of Fibrin Matrix
Because no anticoagulant is used, natural clotting begins as soon as the blood contacts the tube wall.
Fibrinogen (a soluble plasma protein) is converted into fibrin, forming a 3D mesh that traps platelets and white blood cells.
3. Sustained Release of Bioactive Molecules
Inside this fibrin scaffold, platelets gradually degranulate — releasing growth factors like PDGF, TGF-β, VEGF, EGF, and IGF.
Platelet-Derived Growth Factor (PDGF): Stimulates cell proliferation and angiogenesis (new blood vessel formation).
Transforming Growth Factor-beta (TGF-β): Regulates inflammation and promotes collagen synthesis.
Vascular Endothelial Growth Factor (VEGF): Encourages new capillary growth, improving oxygen and nutrient supply.
Epidermal Growth Factor (EGF): Enhances cell turnover and tissue remodeling.
Insulin-Like Growth Factor (IGF): Supports fibroblast activity and extracellular matrix production.
This creates a slow, sustained release of regenerative molecules over several days, stimulating angiogenesis, collagen synthesis, and cellular repair.
PRF mimics the body’s natural wound-healing cascade, providing a biologically active scaffold that supports tissue regeneration and long-term rejuvenation.
4. Healing & Results
The healing process after PRF follows the same biological stages as natural tissue repair, but with enhanced speed and quality due to the prolonged presence of growth factors and fibrin support.
Because PRF releases growth factors slowly, healing tends to be smoother, with less inflammation and downtime than PRP.
Inflammatory Phase (0-3 days)
- Fibrin clot formation, platelet activation, immune cell recruitment
- Mild redness or swelling, natural healing response
Proliferative Phase (3-14 days)
- Fibroblast activity, collagen synthesis, angiogenesis
- Improved texture, firmness, early regeneration
Re-modelling Phase (2-12 weeks)
- Collagen maturation, elastin realignment, dermal thickening
- Visible tightening, rejuvenation, and glow
Extended Re-modelling (3-6 months)
- Continued collagen remodelling and microvascular growth
- Long-lasting aesthetic improvement
Platelet Concentration
Whole blood typically contains 150,000–350,000 platelets/µL.
PRF concentrates this by approximately 2–3 times the baseline count — slightly less than PRP, but more physiologically active because of the inclusion of white blood cells and fibrin.
Importantly, PRF also contains circulating stem cells and cytokines, enhancing regenerative potential.

Active Phase
PHASE 1: Immediate
PRF’s activation begins immediately as the clot forms — there’s no chemical activator added.
Platelet degranulation occurs naturally and continuously within the fibrin matrix.
Growth factor release pattern: ~30–40% of total growth factors are released in the first 24 hours
PHASE 1: Sustained release
- The remaining growth factors are released gradually over 7–10 days
This sustained bioactivity gives PRF a longer regenerative window compared to PRP, which releases most of its growth factors in the first few hours.
TISSUE REMODELING:
Can work from anywhere between 2 weeks-6 months post treatment.
- Collagen formation and aesthetic improvements take place in this phase.
Hair
Mechanism: Increases microvascular supply and activates hair follicle stem cells.
Benefits
Encourages new hair growth
Reduces shedding and miniaturisation
Prolongs the hair growth phase
Most suitable for alopecia patches or bald spots
Skin
Mechanism: Regulates fibroblast activity and collagen re-modelling.
Benefits
Smooths acne scars and surgical scars
Refines texture and pigmentation
- Most suitable for targeted areas of scar/pigmentation/fine lines
Under-eyes
Mechanism: Restores dermal density and vascularity in thin periorbital skin.
Benefits
Reduces dark circles and crepey texture
Firms and thickens delicate under-eye tissue
Lips
Mechanism: Increases microvascular supply and collagen re-modelling.
Benefits
- Natural-looking volume enhancement
- Improved hydration
- Improved pigmentation
- Smoothens texture
Growth-Factor Concentrate (GFC) represents the third generation of autologous platelet therapy, evolved from PRP (Platelet-Rich Plasma) and PRF (Platelet-Rich Fibrin).
It’s designed to deliver pure growth factors without cellular components like red blood cells or white blood cells — resulting in cleaner, more stable, and controlled regenerative action.
GFC contains concentrated levels of:
PDGF (Platelet-Derived Growth Factor) – promotes cell proliferation and angiogenesis
VEGF (Vascular Endothelial Growth Factor) – stimulates new blood vessel formation
EGF (Epidermal Growth Factor) – enhances cellular turnover and repair
TGF-β (Transforming Growth Factor Beta) – regulates inflammation and collagen remodeling
IGF (Insulin-Like Growth Factor) – supports fibroblast activity and tissue renewal
Unlike PRP or PRF, which rely on the gradual release of these factors inside the body, GFC already contains freely available growth factors that act immediately upon injection.
This means GFC is a “pre-activated” biological serum that bypasses the variability of platelet activation inside the body — ensuring consistent, pure, and potent regenerative action.
1. Injection and Local Distribution
When GFC is injected into the scalp or dermal layers of the skin, it immediately disperses through the extracellular spaces around cells.
Because it’s an autologous product (from your own blood), the body does not reject or react negatively to it.
Tiny microinjections deliver it close to the target cells — hair follicle stem cells in the scalp, or fibroblasts and keratinocytes in the skin.
Growth factors start binding to specific receptors on these cells within minutes.
2. Cellular Signalling Activation
Once the growth factors bind to their receptors, a cascade of intracellular signaling pathways is activated — particularly:
MAPK/ERK pathway → promotes cell proliferation (growth and division)
PI3K/Akt pathway → enhances cell survival and reduces apoptosis (cell death)
JAK/STAT pathway → regulates growth-related gene expression
These pathways switch on genes responsible for regeneration, angiogenesis, and collagen synthesis.
3. Biological Effects:
Scalp
- Growth-Factors EGF, IGF, PDGF → Reactivation of dormant follicles → hair enters the anagen (growth) phase
Increased blood supply via VEGF → improved oxygen and nutrient delivery
Stronger, thicker hair shafts from IGF and PDGF stimulation
Reduced follicular miniaturization (the shrinking process seen in hair loss)
Skin
- Growth Factors EGF, IGF, PDGF → Fibroblast stimulation → boosts collagen and elastin production (firmer skin)
Angiogenesis → new micro-vessels improve oxygenation and complexion
Keratinocyte proliferation → improved skin texture and barrier repair
Reduced inflammation due to absence of leukocytes (compared to PRP)
Accelerated healing of micro-injuries
4. Healing & Results
Because GFC delivers ready-to-act growth factors, healing begins almost instantly after application. By being leukocyte-free, it also has an anti-inflammatory effect resulting in smoother healing & minimal irritation.
Growth factors have a short half-life but long-lasting effects because they trigger internal cell regeneration cycles.
The regenerative cascade unfolds through natural biological stages:
Immediate Phase (0-48 hours)
- Direct bio-stimulation of fibroblasts and endothelial cells; increased vascular permeability and nutrient delivery
- Mild redness, warmth, or tightness as cellular metabolism increases
Sustained Phase (3-14 days)
- Collagen synthesis, angiogenesis, and extracellular matrix production
- Early improvement in skin tone, hydration, and elasticity
Re-modelling Phase (2-12 weeks)
- Maturation of collagen fibres and dermal restructuring
- Visible firming, texture refinement, reduction in wrinkles or hair shedding
For scalp, visible hair improvement usually appears after 2–3 sessions (about 2–3 months).
Growth-Factor Concentration
GFC is derived from platelets but does not contain intact platelets; only the released growth factors are retained.
The process yields up to 5–10× the concentration of growth factors found in normal plasma, depending on the preparation kit used.
Platelet Count: Since the platelets are lysed during processing, there’s no measurable platelet count — what matters is the growth factor density, which is substantially higher and immediately bioavailable.

Active Phase
PHASE 1: Immediate (within minutes post-injection)
Growth factors bind to cell receptors, initiating signalling pathways for tissue repair and angiogenesis.
PHASE 2: Sustained Release (1-14 days)
Continuous stimulation of fibroblasts, keratinocytes, and stem cells to produce collagen, elastin, and new capillaries.
TISSUE REMODELING (2-12 weeks):
Structural strengthening and collagen maturation; visible, lasting rejuvenation.
Hair
Mechanism: Growth factors stimulate dermal papilla cells, promote angiogenesis, and re-awaken dormant follicles.
Benefits
Reduces hair fall
Increases hair thickness and density
Enhances scalp circulation and follicle nutrition
Timeline: Reduced shedding within 3–4 weeks; visible regrowth in 2–3 months.
Skin
Mechanism: Activates fibroblasts and increases dermal matrix turnover.
Benefits
Improves skin texture, elasticity, and hydration
Reduces fine lines, wrinkles, and pores
Promotes a brighter, more even skin tone
Scars
Mechanism: Accelerates fibroblast proliferation and collagen reorganisation.
Benefits
Smoother skin surface and improved scar texture
Reduction in post-inflammatory hyperpigmentation
Better overall dermal uniformity
Under-eyes
Mechanism: Boosts microcirculation and collagen in periorbital skin.
Benefits
Decreases dark circles and fine lines
Improves firmness and skin thickness under the eyes
Platelet-derived Exosomes (PLT-Exos) represent the next frontier in regenerative and cellular aesthetics — an advanced evolution beyond PRP, PRF, and GFC.
While PRP and PRF rely on platelets to release growth factors directly, PLT-Exos isolates the pure extracellular vesicles (exosomes) secreted by activated platelets. These nano-sized messengers (30–150 nanometers) carry potent regenerative instructions to target cells, stimulating tissue healing, collagen production, and hair follicle activation at a molecular level.
PLT-Exos are extracellular vesicles released by almost all cells, including activated platelets. They carry bioactive cargo such as:
mRNA and microRNA (miRNA) – regulate gene expression in target cells
Proteins and peptides – including growth factors, enzymes, and adhesion molecules
Lipids – maintain vesicle stability and aid in cell signalling
These signals are specifically enriched with platelet-derived growth factors and regenerative molecules.
Because they can enter recipient cells directly, PLT-Exos delivers precise biological instructions, stimulating rejuvenation and tissue homeostasis without introducing whole cells.
1. Isolation and Preparation
Blood is drawn and processed using a specialized multi-step centrifugation and filtration system.
Platelets are activated to release exosomes, which are then purified to create a concentrated, cell-free solution rich in platelet-derived nanovesicles.
2. Local Distribution
When platelet-derivedexosomes are injected into the scalp or dermal layers:
They diffuse easily through the extracellular matrix (because of their tiny size).
They are taken up by nearby cells — mainly:
Dermal papilla cells (in the scalp)
Hair follicle stem cells
Fibroblasts (in the skin)
Keratinocytes and endothelial cells
They enter these target cells via endocytosis — a process where the cell “engulfs” the exosome to absorb its contents.
3. Cellular Uptake & Signal Delivery
Once inside the cell, exosomes release their cargo (growth factors, RNA, and proteins) directly into the cytoplasm.
This triggers several intracellular signalling pathways, such as:
PI3K/Akt pathway → promotes cell survival and metabolism
MAPK/ERK pathway → enhances cell proliferation and differentiation
Wnt/β-catenin pathway → crucial for hair follicle activation
TGF-β/Smad pathway → modulates collagen production and reduces scarring
These pathways reprogram local cells to behave more like active cells again.
4. Effects
Because PLT-Exos is cell-free, it eliminates variability in platelet counts and clotting factors. Instead, it delivers precisely concentrated signalling molecules — the pure bioactive essence of regenerative platelet therapy.
Scalp
Activate dormant follicles
→ Growth factor signals restart the anagen (growth) phase of hair.Stimulate dermal papilla cells
→ Increases production of keratin and extracellular matrix — leading to thicker, healthier hair.Promote angiogenesis
→ VEGF encourages new capillaries to form around follicles, improving oxygen and nutrient delivery.Reduce inflammation
→ Exosomes contain anti-inflammatory cytokines that calm the scalp environment, preventing further follicle damage.
Skin
Stimulate fibroblasts
→ Boosts production of collagen I & III, elastin, and hyaluronic acid, improving firmness and elasticity.Enhance angiogenesis
→ New blood vessel growth improves skin tone, texture, and healing.Regulate pigmentation
→ Some exosomal miRNAs suppress excess melanin synthesis, leading to a more even skin tone.Accelerate healing and reduce inflammation
→ Exosomes help close micro-wounds faster
5. Healing & Results
PLT-Exos initiates cellular communication and repair immediately, but tissue re-modelling continues for weeks as the molecular effects cascade through target tissues.
Immediate Phase (0-48 hours)
- Exosomes bind to surface receptors on fibroblasts, keratinocytes, and stem cells; intracellular signalling (via mRNA and miRNA) begins.
- Mild warmth or redness; early hydration and glow.
Sustained Phase (3-14 days)
- Up-regulated synthesis of collagen, elastin, and hyaluronic acid; angiogenesis and cellular detoxification.
- Noticeable improvement in texture and tone; skin looks firmer and fresher.
Re-modelling Phase (2-12 weeks)
- Long-term gene modulation supports collagen maturation, dermal thickness, and vascular stability.
- Visible tightening, refined texture, and improved elasticity.
Platelet Concentration
PLT-Exos is derived from platelets, but no intact platelets remain — only purified exosomes and their growth factor cargo.
Exosome Concentration: Each PRX preparation may contain billions of exosomes per milliliter, carrying high concentrations of PDGF, VEGF, TGF-β, EGF, and IGF, as well as microRNAs that regulate collagen and hair follicle gene expression.

Active Phase
PLT-Exos begins acting immediately, but its molecular signalling continues for several days, as target cells translate exosomal RNA into new proteins that remodel tissue over time.
PHASE 1: Immediate (0-48 hours)
Exosomes integrate with target cells; initiate regenerative signalling.
PHASE 2: Sustained Release (3-14 days)
Collagen, elastin, and capillary formation; anti-inflammatory cytokine release.
TISSUE REMODELING (2-12 weeks):
Structural tissue renewal and long-term cellular optimisation.
Hair
Mechanisms: PLT-Exos target dermal papilla cells in hair follicles, delivering mRNA and proteins that activate growth-phase genes. They also improve microvascular blood flow and modulate inflammation around follicles — two critical factors in hair regeneration.
Benefits
Stimulates new hair growth by reactivating dormant follicles
Prolongs the anagen (growth) phase of the hair cycle
Reduces shedding and follicular miniaturization
Thickens existing hair shafts and improves overall density
Enhances scalp circulation and oxygenation
Results
Reduced hair fall: 2–4 weeks
Visible new growth: 8–12 weeks
Optimal density and thickness: 3–6 months
Skin
Mechanisms: Exosomes stimulate fibroblasts, keratinocytes, and endothelial cells, triggering controlled regeneration and microvascular repair.
Benefits
Improves skin tone, firmness, and elasticity
Reduces fine lines, wrinkles, and enlarged pores
Restores hydration and radiance through enhanced extracellular matrix quality
Decreases inflammation and oxidative stress (ideal for sensitive or rosacea-prone skin)